Fréttamiðlar í Ástralíu og í Bandaríkjunum verið staðnir að því nota sömu ljósmyndirnar í fréttaskýringum sínum en ljósmyndirnar eru sagðar vera af ákveðnum einstaklingum með nýleg “apabóluútbrot“.
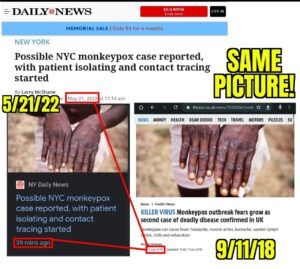



- Komið hefur í ljós að um er að gamlar ljósmyndir sýna “ristilútbrot” framan á handarbaki manneskju með húðsjúkdóminn Ristil (Herpes zoster) sem eru sársaukafullar smáblöðrur af völdum hlaupabólu-ristilveiru (Varicella zoster veiru) og er um endurvakningu á hlaupabóluveirunni að ræða, venjulega mörgum árum eftir upprunalegu sýkinguna.

Á færslu Þórólfs Guðnasonar á vef Embættis landlæknis segir að sjúkdómur sé orsakaður af veiru sem sé náskyld bólusóttarveiru (orthopox) og sé einkum þekktur hjá dýrum en einnig mönnum.
Smit frá dýrum til manna séu sjaldgæf og sömuleiðis smit milli manna.
Hefðbundin viðbrögð í fyrstu en svo komu útbrotin
Stella Jórunn A. Levy sjúkraliði fékk vel upphleypt útbrot um bringu og háls með tilheyrandi verk, kláða og sviða eftir bólusetningu. Hún telur víst að bóluefnið hafi vakið vírusinn.

„Nóttina á eftir var ég lasin með hita, beinverki og höfuðverk.“ Stella segir það dæmigerð viðbrögð við bólusetningu en hún var svo einkennalaus með öllu um miðjan næsta dag fyrir utan eymsli í hnakka og herðum.
Janúar 2022 – Pfizerog BioNTech hyggjast þróa saman bóluefni gegn ristli eftir vel heppnað samstarf við Covid-19 bóluefnið.

Þýska líftæknifyrirtækið BioNTech og bandaríski lyfjarisinn Pfizer hyggjast starfa saman til að þróa mRNA bóluefna gegn smitsjúkdómnum ristli (e. shingles) og fara þar með í samkeppni við flaggskip breska lyfjafyrirtækisins GlaxoSmithKline (GSK). Financial Times greinir frá.
BioNTech og Pfizer vonast til að endurtaka vel heppnað samstarf við þróun á bóluefni gegn Covid-19. Þar hefur BioNTech útvegað mRNA tækni sem þýska fyrirtækið er með einkaleyfi á, og Pfizer ræðst í rannsóknir á mótefnavökum (e. antigen). Pfizer hafði áður gefið í skyn að það myndi hefja þróun á mRNA bóluefnum á eigin vegum.
Pfizer malar gull á bóluefni og hækkar afkomuspár
Sjá einnig: Tekjur borgarinnar margfaldast út af Covid
Fjárfesting bóluefnaframleiðenda í mRNA hefur aukist verulega eftir að tæknin nýttist gegn Covid-farsóttinni. Mörg fyrirtæki horfa til sjúkdóma sem ekki er búið að þróa bóluefni gegn eða þar sem fyrri bóluefni voru ekki mjög áhrifarík, líkt og með inflúensuna.
Pfizer og BioNTech ákváðu þó að horfa til ristils, jafnvel þó GSK fékk bóluefni samþykkt gegn sjúkdómnum árið 2017. Bóluefni GSK, Shingrix, veitir meira en 90% vörn en breski lyfjaframleiðandinn hefur hins vegar átt í erfiðleikum með að auka framleiðslu sína til að anna eftirspurn. Pfizer og BioNTech vonast til að auðveldara verði að skala upp framleiðslu á bóluefni sem byggt er á mRNA tækninni.
Sala á Shingrix bóluefninu nam 502 milljónum punda á þriðja fjórðungi 2021, sem er 34% aukning frá sama tímabili árið áður.
Um einn af hverjum þremur Bandaríkjamönnum fær ristil í gegnum ævina. Ristill eru sársaukafullar smáblöðrur af völdum hlaupabólu-ristilveiru.
Búið ykkur undir næsta heilaþvott, fjöldabólusetningar áróður í boði mútuþægra meginstraumsfjölmiðla sem verður rúllað út á næstunni 

Monkeypox was first identified in 1958 in colonies of monkeys, and the first human case of the virus was identified in 1970 in the Democratic Republic of the Congo. Most likely this was just the first case identified, as people living in Africa have been in contact with monkeys and the other Monkeypox animal hosts for millennia. The “West African” monkeypox clade (clade = variant) circulating outside of Africa at this time causes a milder disease compared to the closely related virus found found in other regions of Africa (Congo clade).
The symptoms of monkeypox are somewhat similar to, but much milder than smallpox disease. The general clinical presentation of the disease caused by the West African monkey pox clade virus involves Influenza-like symptoms — fever, body aches, chills — together with swollen lymph nodes. A rash on the palm of the hand is often observed. In the latter stage of the disease, which may last for up to a month or more in some cases, may involve small lesions which develop a crust, and which can result in a small depigmented scar. There is no evidence of asymptomatic transmission. In other words, current medical knowledge indicates that it is only spread by person to person contact between an uninfected individual and someone who already has symptoms of the disease. Therefore, disease spread can be readily controlled by classical public health interventions such as contact tracing, temporary quarantine of those who have had physical contact with someone who is infected, and longer term quarantine of those who develop symptoms. Essentially all of the current cases in the west which we are seeing in the news are among men who have sex with men, and appear to be due to close physical contact. Monkeypox is endemic in many parts of Africa, and is a “zoonotic” virus, meaning it can be transmitted from a variety of animals (not just monkeys) to humans. Initial animal to human transmission followed by limited human to human transmission is probably the cause of the sporadic cases typically observed in Africa. Chicken pox, which is highly transmissible, is not part of the genus Orthopoxvirus, despite that name “pox.” Once again for emphasis, Cowpox and Camelpox are also in the genus Orthopoxvirus, and they are not particularly pathogenic when contracted by humans; just because Monkeypox is a “pox” virus in the genus Orthopoxvirus, does not mean it is particularly deadly.
Monkeypox is a double stranded DNA virus, which means that due to the double stranded nature of DNA each of the two strands act as a “check” on the other during replication. As a consequence of this “error checking”, this and other DNA viruses mutate much more slowly than RNA viruses do. Over time, DNA virus genomes are relatively stable. This means that, unlike SARS-CoV-2 (COVID) or influenza, Monkeypox is unlikely to rapidly evolve to escape either naturally acquired or vaccine induced immunity. For the purposes of making a vaccine, this makes it a much easier target that say, a rapidly evolving RNA Coronavirus such as SARS-CoV-2, the virus which causes COVID-19. Furthermore, from an immunological point of view, the various Orthopox viruses often are cross-protective. In other words, if you have been vaccinated with a smallpox vaccine, or previously infected by Cowpox, Camelpox, or Monkeypox, you are highly likely to be quite resistant to disease caused by the Monkeypox virus which is now being (quite rarely) reported in non-African countries.
Current data indicate that Monkeypox is not very infectious in humans – it has a low Ro (perhaps below 1), which is the term used to describe how efficiency an infectious disease can spread from human to human. Again, this is super good news for containment. An Ro of <1 generally means that (even in the absence of social distancing of other containment measures), for every person already infected, on average less than one other person will become infected. For comparison purposes, the Omicron variants of SARS-CoV-2 have an Ro in the range of 7 to 10. A virus with an Ro of less than one can be easily contained with the standard public health methods discussed above. A virus with an Ro of 7-10 essentially cannot be contained and will rapidly spread throughout the world, as we have seen with the Omicron variants. In the case of a virus with an Ro around 1 or less, traditional infectious disease containment methods such as contact tracing, identification and isolation of infected individuals can be all that is needed to control the virus. Now the fact that Monkeypox is being spread from human to human (rather than only arising from contact between a person and an infected animal) is not such good news, but since this transmission appears to be from very close contact, this means that it can be easily contained without resorting to a general population vaccination campaign. In this type of setting, if there is a significant outbreak, vaccination is often restricted to just the health care and/or first responder personnel most likely to be in contact with an infected person. Using a vaccine to help that containment via either “ring” vaccination or wide-spread vaccination strategies is generally unnecessary, and may even be counterproductive, depending on the safety of the vaccine – keeping in mind that no drug or vaccine is perfectly safe.
Let me take a moment to tell a personal story to illustrate this point. After the 9-11 events including the anthrax letters, I took a job involving clinical development of a wide range of biodefense vaccines under a US Department of Defense (DoD) contract (issued to Dynport Vaccine Company). One of the vaccine indications we worked on was for prevention of Smallpox. The Vice President of the United States at the time, Mr. Dick Cheney, was advocating for widespread vaccination against smallpox because it was thought that there was something like a 1% chance of a bioterror attack involving reintroduction of smallpox into the United States. The existing live attenuated smallpox vaccine began to be deployed throughout the United States to healthcare workers and first responders. Then multiple reports of vaccine-caused damage began to circulate. I was tasked with looking into historic DoD smallpox vaccine campaign records concerning these types of “adverse events”. Adverse events after administration of this live attenuated vaccine were well known, and generally fell into two categories. In some cases, a small subset of young warfighters and recruits had some previously undetected immunologic defect which resulted in them developing an ongoing infection by the live attenuated vaccine virus that was being used at the time. The other group developed more subtle symptoms including what now appears to have been vaccination-associated myo- and pericarditis – typically ascribed to an autoimmune process. These problems were known risks back when smallpox vaccination was common (and smallpox had not been eradicated) and therefore no surprise when the same vaccine was redeployed in the present. But smallpox had been eradicated, and Mr. Cheney’s worst case scenario never happened. Those who were vaccinated and damaged to protect against a non-existent threat provide a great example illustrating a completely upside down risk benefit ratio. All risk, no benefit. And, appropriately, the smallpox vaccination campaign was halted.
Key takeaway: this is not influenza or COVID – this virus mutates slowly, it is not highly infectious, naturally acquired immunity is potent and long lasting, and Orthopox vaccines are usually cross protective. The risk of immunologic escape is very, very low. And the spread of this virus can be readily stopped by simple, inexpensive classical public health measures. If it were otherwise, we would already have experienced a pandemic of Monkeypox decades ago.
Monkeypox disease severity can vary with different clades (found in different regions in Africa, which also suggest the virus has been around for a very long time). Luckily, this particular clade is less severe and appears to be endemic in Africa. Unfortunately, it has rarely been studied and so relatively little is known about the virus and associated human disease, largely because the infectious threat to the general population is so low. STAT news’ journalist Helen Branswell has recently interviewed CDC experts, and published an excellent summary of the clinical presentation:
“With one to three days of the onset of fever, a distinctive rash appears, often starting on the face. Many conditions can cause rashes but the monkeypox rash has some unusual features, notably the fact that vesicles can form on the palms of the hands. In countries where it is endemic, the virus is believed to mainly spread to people from infected animals when people kill or prepare bushmeat for consumption.
Once the virus jumps to people, human-to-human transmission can occur via respiratory droplets — virus-laced saliva that can infect the mucosal membranes of the eyes, nose, and throat — or by contact with monkeypox lesions or bodily fluids, with the virus entering through small cuts in the skin. It can also be transmitted by contact with clothing or linens contaminated with material from monkeypox lesions. (STAT News).
There was a prior outbreak of Monkeypox in the United States during 2003. That particular outbreak, the first reported outside of Africa, was traced back to the importation of small mammals from Ghana. As shown by this outbreak, multiple animals can contract the disease – during that outbreak, giant pouched rats and squirrels tested positive for the virus and eventually spread it to prairie dogs being sold as pets in multiple Midwestern states (per the CDC). Forty-seven people caught the disease from the prairie dogs. This is important and relevant history, because the current outbreak appears to be occurring from human to human transmission, with no single individual traced as as case zero. There have been a few other outbreaks outside of Africa over the years from travelers coming from Nigeria. It is currently thought that the Monkeypox virus is much more common in Nigeria than has previously been reported.
There is a vaccine that was licensed in the U.S. in 2019 for people 18 years of age
and older to protect against smallpox and monkeypox; Bavarian Nordic’s Jynneos. A second vaccine, ACAM2000 made by Emergent Product Development, protects against smallpox and is also thought to offer some protection against monkeypox. Both vaccines are licensed only for people considered at high risk of contracting the disease because they are not entirely safe. In the 2003 Monkeypox outbreak in the U.S., smallpox vaccine was deployed to persons considered at high risk.
The U.S. already holds supplies of the vaccines in the Strategic National Stockpile, a hedge against public health emergencies. “To combat a smallpox emergency, the SNS holds enough smallpox vaccine to vaccinate the entire U.S. population. In addition, the SNS has antiviral drugs that can be deployed to treat smallpox infections, if needed,” a spokesperson for the Department of Health and Human Services said via email. In my opinion, the 119 Million dollar smallpox vaccine purchase which was just authorized by the US HHS and Biden administration represents an unnecessary and unwarranted expense, unless there are data showing that the current strain is significantly different from the historic predecessor strains within this clade.
The WHO’s Van Kerkhove noted that some of these products have been licensed using what is known as the animal rule, where animal efficacy data are used as a surrogate because the lack of circulating smallpox means the vaccines or drugs can’t be tested for efficacy in people. As a result, any such product could only be used in the context of a clinical trial, she said.
“There are options. We just have to make sure that they’re used appropriately. One of the things related to vaccines is we want to make sure if the vaccines are needed and used, they’re used among populations that need them the most. There’s not ample supply of anything right now,” she said.
Still, she expressed confidence the outbreak can be controlled.
“What we need to do right now is focus on stopping the spread. And we can do that. We can do that with the appropriate messaging, with the appropriate testing … with supportive isolation and clinical care as necessary, with protecting health workers,” Van Kerkhove said. (STAT News).
The Bill Gates funded organization GAVI has provided their assessment of the medical threat posed by Monkeypox, which can be found here. Many readers of this substack will not be surprised by my assessment that this GAVI threat assessment is highly biased towards overstatement. For example, the article seeks to create parallels between Monkeypox and Ebola:
Similar to viruses like Ebola, transmission only happens in close proximity by contact with lesions, body fluids, respiratory droplets or contaminated materials such as bedding or clothes.
The article also states the following pants-on-fire disinformation;
Although symptoms often ease within a month, one in ten cases can be fatal. Children are particularly susceptible.
Factcheck determination by qualified subject matter expert –
This assertion represents a very biased interpretation of a data report from the World Health Organization:
In 2020, the World Health Organization (WHO) reported 4,594 suspected cases of monkeypox, including 171 deaths (case fatality ratio 3.7%). They are described as suspected because confirmation requires PCR testing, which is not easily available in endemic areas.
Those readers who have become sensitized to this type of information manipulation and weaponization will immediately notice two key things about this comment. First, the reported mortality of 3.7% (NOT 10%) of cases is from suspected, not confirmed cases. Secondly, this type of sampling is highly biased towards more severe disease- countries rarely will detect and do not report cases of mild disease to the WHO.
So, is the biothreat real? Is is imminent? Does it justify the global media hype? As I was waiting in an airport lounge to travel from USA to the UK two days ago, I saw a newsreel from CNN which was breathlessly reporting on this “threat” while displaying historic images of patients suffering from Smallpox disease. This provides a classical example of public health fearporn, in my opinion, and CNN should be reprimanded for broadcasting irresponsible propaganda – misinformation and disinformation- under the guise of journalism.
In my opinion, based on currently available information, Monkeypox is a virus and disease which is endemic in Africa, emerges sporadically after transmission into humans from animal hosts, and is typically spread by close human contact. It is readily controlled by classical public health measures. It does not have a high mortality rate. Unless there has been some genetic alteration, either through evolution or intentional genetic manipulation, it is not a significant biothreat, and has never been considered a high threat pathogen in the past.
So stop the fear mongering, misinformation and disinformation.
Um höfund

- Sigurlaug Ragnarsdóttir
- ✞༺(((( Ⓒilla ℜągnąℜṧ )))༻♚༺ BA Classical Art Historian || MA Culture & Media || Tourism & Sales Management || Web Design || Photo & Videographer for Tourism Magasins ༻
Síðustu færslur
 PROTECT THE CHILDREN23. nóvember, 2024BARNAMÁLARÁÐSTEFNAN 2024
PROTECT THE CHILDREN23. nóvember, 2024BARNAMÁLARÁÐSTEFNAN 2024 MANNRÉTTINDI19. nóvember, 2024MENNTASPJALL VALGERÐAR SNÆLAND JÓNSDÓTTUR
MANNRÉTTINDI19. nóvember, 2024MENNTASPJALL VALGERÐAR SNÆLAND JÓNSDÓTTUR Sigurlaug Ragnarsdóttir15. ágúst, 2024‘Really Chilling’: Five Countries to Test European Vaccination Card
Sigurlaug Ragnarsdóttir15. ágúst, 2024‘Really Chilling’: Five Countries to Test European Vaccination Card MANNRÉTTINDI9. ágúst, 2024Lög um borgaralega handtöku voru felld úr gildi árið 2008
MANNRÉTTINDI9. ágúst, 2024Lög um borgaralega handtöku voru felld úr gildi árið 2008