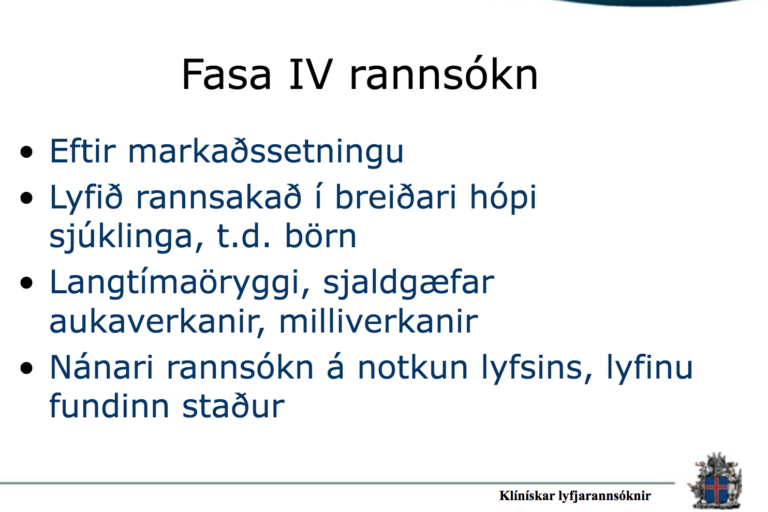
Considerations regarding consent in vaccinating children and adolescents between 6 and 17 years old
Around the world, immunization programmes are increasingly including, in their national immunization schedules, vaccines that target age groups beyond infancy and early childhood. This document is aimed at programme managers who are
planning to introduce vaccines for older children and adolescents aged between 6 and 17 years.1 It provides information that should be considered when preparing guidance notes on the consent process, or for clarifying questions from the health
workers who provide the vaccinations. The document is all the more important because this population group may present for vaccination without an accompanying parent or legal guardian.
Introduction
1. According to the Convention on the Rights of the Child (1989), childhood ends upon reaching 18 years of age. In most countries in the world, this is often considered the age at which legal adulthood, the age of majority, is reached.
The principles of consent and assent
Consent
Consent is the principle wherein individuals must give their permission before receiving a medical intervention or procedure. According to the laws and regulations in place in most countries, consent is required for a range of medical interventions
or procedures, from a simple blood test to organ donation, and including vaccinations. In only very few, well-described circumstances, such as lifethreateening emergencies, may consent be waived.
Consent derives from the principle of autonomeyand forms an important part of medical and public health ethics, as well as international law.2
For consent to be valid, it must be informed, understood and voluntary, and the person consenting must have the capacity to make the decision.
Assent
Assent refers to the process of children’s and adolescents’ participation in the decision-making on vaccination (or other medical interventions). Assent is not regulated in law like consent, and is sometimes referred to as a moral obligation closely linked to good practice in dealing with patients. International law provides strong support for children’s rights to participate in decisions about their health and health care, and also in the planning and provision of health services relevant
to them and based on their evolving capacity.3
2. Convention on the Rights of the Child, General Comment No. 4 (CRC/C/GC/4, 1 July 2003) and No. 15 (CRC/C/GC/15, 17 April 2013).
- 3. CRC/C/GC/4, 1 July 2003 states that “adolescents need to have a chance to express their views freely and their views should be given due weight, in accordance with article 12 of the Convention.”
- © Ammad Khan
- 3 Common approaches for obtaining consent for vaccination
1. A formal, written consent process is used, particularly in middle- and high-income countries that have a higher percentage of literate populations and a longer history of providing vaccination to older age groups.
4 Vaccination of this target group may be delivered through school health services. Health authorities inform the parents about the vaccination and written consent from the parent is required to opt-in, i.e.give permission for the older child/adolescent
to be vaccinated. Alternatively, a written form isused to allow parents to express non-consent (or refusal) to vaccination of their child. This is known as an opt-out procedure.
2. A verbal consent process, whereby consent is given verbally by the parent after being duly informed about the vaccination. However, this approach can only be used when parents accompany the child to the vaccination.
3. An implied consent process by which parents are informed of imminent vaccination through social mobilization and communication, sometimes including letters directly addressed to the parents. Subsequently, the physical presence of the child or adolescent, with or without an
accompanying parent at the vaccination session, is considered to imply consent. This practice is based on the opt-out principle and parents who do not consent to vaccination are expected implicitly to
take steps to ensure that their child or adolescent does not participate in the vaccination session.
This may include not letting the child or adolescent attend school on a vaccination day, if vaccine delivery occurs through schools.
Implied consent procedures are common practice in many countries. However, when children present for vaccination unaccompanied by their parents, it is challenging to determine whether parents indeed provided consent. Therefore, countries
are encouraged to adopt procedures that ensure that parents have been informed and agreed to the vaccination. Comprehensive data on whether the approach countries use to deal with consent has changed or evolved over the last decades is
not available.
Approaches to obtain informed consent:
1. Written consent
2. Verbal consent
3. Implied consent
4. A WHO survey in 2012 in 34 selected countries from four regions on consent procedures for vaccination in 6–17 year-olds, found that approximately half of the respondent countries use written consent for vaccination in this age group.
Current practices of obtaining informed consent for vaccination vary among countries, but can be broadly categorized into three approaches.
© C. McNab
4. Schools and communities can authorize, not give consent Mandatory vaccination does not always overrule the need for consent
- Based on concepts of vaccines as a public good, or on public-health goals of disease elimination and outbreak control, some countries identify one or more vaccines as mandatory in law, or in their policies. Vaccination may, for example, be made a condition for entry into preschool or primary school, or to enable access to welfare benefits. Whether consent is needed for mandatory vaccination depends on the legal nature of the regulations. When mandatory vaccination is established in relevant provisions in law, consent
may not be required. If the mandatory nature of - vaccination is based on policy, or other forms of soft law, informed consent needs to be obtained as for any other vaccines. Some countries allow individuals to express non-consent (opt-out) and
obtain an exemption for mandatory vaccines. - This may come with certain conditions, like barring unvaccinated children from attending school during disease outbreaks…..
Um höfund

- Sigurlaug Ragnarsdóttir
- ✞༺(((( Ⓒilla ℜągnąℜṧ )))༻♚༺ BA Classical Art Historian || MA Culture & Media || Tourism & Sales Management || Web Design || Photo & Videographer for Tourism Magasins ༻
Síðustu færslur
 PROTECT THE CHILDREN23. nóvember, 2024BARNAMÁLARÁÐSTEFNAN 2024
PROTECT THE CHILDREN23. nóvember, 2024BARNAMÁLARÁÐSTEFNAN 2024 MANNRÉTTINDI19. nóvember, 2024MENNTASPJALL VALGERÐAR SNÆLAND JÓNSDÓTTUR
MANNRÉTTINDI19. nóvember, 2024MENNTASPJALL VALGERÐAR SNÆLAND JÓNSDÓTTUR Sigurlaug Ragnarsdóttir15. ágúst, 2024‘Really Chilling’: Five Countries to Test European Vaccination Card
Sigurlaug Ragnarsdóttir15. ágúst, 2024‘Really Chilling’: Five Countries to Test European Vaccination Card MANNRÉTTINDI9. ágúst, 2024Lög um borgaralega handtöku voru felld úr gildi árið 2008
MANNRÉTTINDI9. ágúst, 2024Lög um borgaralega handtöku voru felld úr gildi árið 2008